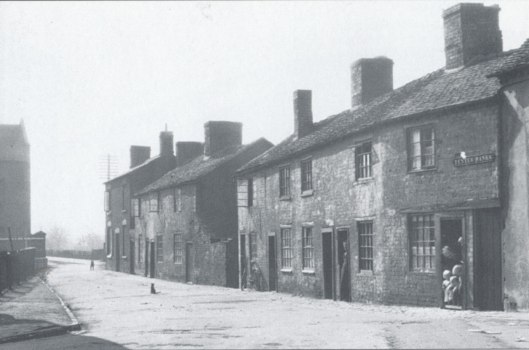
Mavis Bowers was born prematurely on 26th September 1929, at home in Bull Hill Stafford. She had a twin brother David who only lived for a short while. Mum was ‘smaller than a bag of sugar’ when she was born and for the first weeks of her life had to be washed in olive oil, dressed in doll’s clothes and a small drawer was used as a cot. Her birth wasn’t registered for two months.
When the picture of mum and the challenge shield was taken mum was eight months’ old, & still not able to sit up for herself. The wooden “Challenge Shield” was an engraved silver plaque for “Stafford Infant Welfare Centre’s Annual Competition for infants during their first year”. This began in 1920 and ended in 1948 (the year the NHS was set up). Mothers who won were presented with one small shield which they could keep, and the large ‘Challenge Shield’ which they kept for 12 months. They also pushed the baby in a pram along Stafford’s main street at Stafford Pageant. The silver plaque was made by G & S Ltd.
Mavis’s mother Frances Bowers brought up her three daughters on her own. They lived in Prospect Road, Coton Fields, Stafford.

Another picture shows Mum and her older sisters, Olive and Joyce with mum in her dad William Bowers’ arms . Shortly after this my grandad William went into St George’s Hospital, where he remained until he died, about 30 years later. Mum can remember visiting him in the hospital as a young child. She described how there were many doors to unlock and how the attendants (this was before mental health nurses) were very kind to her and her mother.
We now know granddad had some sort of post traumatic illness, although at the time people didn’t talk about it, and it was said he had been ‘gassed in the first world war’. We have now found out that Fabry disease runs in the family (originating on mum’s side). This rare enzyme disorder, which causes limb pain and organ degeneration, has been misdiagnosed as a mental illness in the past. We wonder if that’s what granddad was suffering from.

Mavis and her two sisters brought up in poverty by their mum Frances. Mum remembers her childhood as happy and secure. One of mum’s memories was being sent by her mum to fetch dripping from a local hospital. (Dripping is the fat and juices that come off roast meats.) Mum and her sisters had to take a walk across some fields, where they used to be frightened of the horses, and knock at the kitchen door of the hospital. They then gave a penny for a jug to be filled with dripping. Mum also remembered how her mother used to wash and dry the girl’s school clothes every night, as they only had one set of school uniforms.

Mum’s upbringing made her really appreciative of the small things in life and never to take anything for granted.
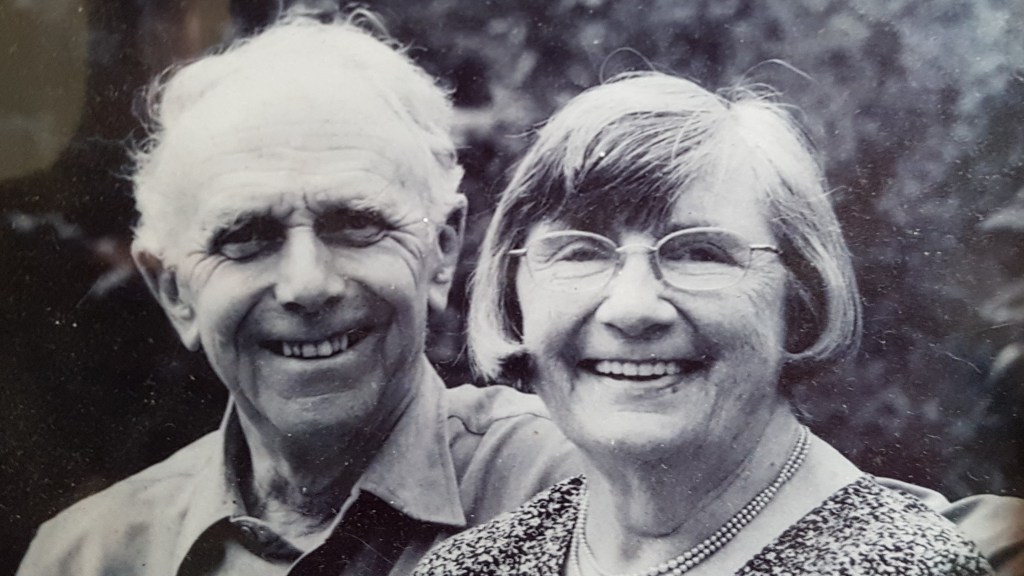
After leaving school at 14 Mavis started training as a seamstress and later worked at Lotus shoe factory. Mavis Bowers married Jim Turner a chartered electrical engineer, originally from Plymouth, who worked at English Electric in Stafford, and went on to have two sons, Steve and Nick. Mavis enjoyed sewing and, after the children left, worked from home as a seamstress. Mavis and Jim enjoyed travel and visited Europe often when they were older. At the age of 70 Mavis also went to Australia on her own and had the holiday of a lifetime travelling from Melbourne to Townsville in north Queensland, visiting friends of her son Steve who have lived there for 5 years. After 59 years of marriage Jim Turner died in 2012.

Mum took up paintings at age 80 and completed several pictures, some abstract and some from memory. The picture above is of Mungo Lakes, where mum visited when she was in Australia.

In the latter years of mum’s life she had glaucoma, osteoporosis Parkinson’s disease and heart failure and was unable to leave the house. Despite this mum remained independent and lived on her own, with carers visiting. This continued until a couple of years before she died, when she had a live-in carer.
For the final months of mum’s life she was cared for by Belinda Comfort Damoah. Belinda stayed with mum for six months, throughout the covid-19 epidemic, and is held in high esteem by mum, all the family and friends.
I was able to spend the final 12 weeks of mum’s life helping look after her at home, where she passed away in July 2020.
Belinda has recently spearheaded the formation of the Akwaama Toprefo Female Club (ATOFEC) which has the education of young women and the skills training of women as it’s objective.
We collected for this project at mum’s funeral, and the family is proud to be linked with such a worthwhile endeavor. Mum’s picture now hangs on the wall of the schoolroom.

Written by Steve Turner Version dated: 14.12.2020
Revisions: Picture of Bull Hill, Stafford added. 25.01.2021
Thanks to Melanie Williamson, Collections Assistant, Staffordshire Archives and Heritage, Staffordshire County Council for finding the shield and providing pictures and information.
Website: http://www.staffordshire.gov.uk/archives
Facebook: http://www.facebook.com/StaffordshireArchivesandHeritage
Twitter: http://www.twitter.com/@ArchandHeritage